A student learns what information about acute pancreatitis? Acute pancreatitis is a serious condition that affects the pancreas, an organ that plays a vital role in digestion. This condition can be caused by various factors, including gallstones, excessive alcohol consumption, and certain medications.
Understanding the causes, symptoms, diagnosis, and treatment of acute pancreatitis is crucial for students in the medical field or anyone seeking to learn more about this important topic.
This guide will delve into the intricacies of acute pancreatitis, providing a comprehensive overview of its causes, symptoms, diagnosis, treatment, and prevention. We will explore the potential complications, the role of nutrition in management, and the importance of patient education and support.
By understanding this information, students can gain valuable insights into this condition and its implications for patient care.
What is Acute Pancreatitis?
Acute pancreatitis is a serious condition that involves inflammation of the pancreas, a gland located in the upper abdomen. This inflammation can cause severe pain, as well as complications that can be life-threatening.
Causes of Acute Pancreatitis
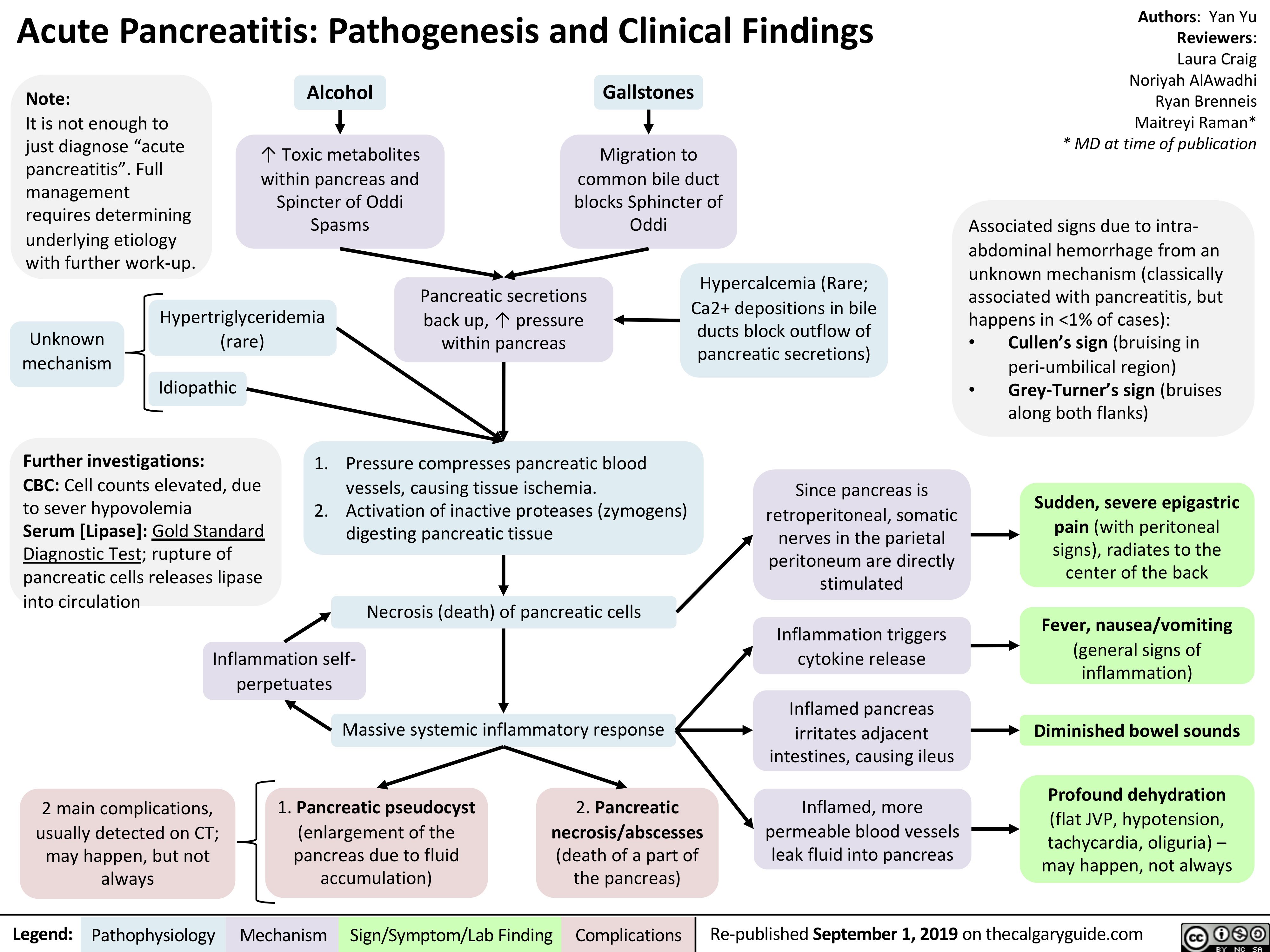
Acute pancreatitis can be caused by a variety of factors. The most common causes are gallstones and alcohol abuse.
Gallstones
Gallstones are small, hard deposits that can form in the gallbladder. When a gallstone blocks the pancreatic duct, it prevents pancreatic enzymes from flowing properly, leading to inflammation and pancreatitis.
Alcohol Abuse
Excessive alcohol consumption can directly damage the pancreas, leading to inflammation and pancreatitis. Chronic alcohol abuse is a significant risk factor for developing pancreatitis.
Other Causes
Other less common causes of acute pancreatitis include:
- High triglycerides: High levels of triglycerides in the blood can also trigger pancreatitis.
- Certain medications: Some medications, such as steroids and certain antibiotics, can increase the risk of pancreatitis.
- Infections: Infections, such as viral infections, can sometimes lead to pancreatitis.
- Trauma: Injury to the abdomen, such as from a car accident, can also cause pancreatitis.
Risk Factors for Acute Pancreatitis
Several factors can increase the risk of developing acute pancreatitis. These include:
Age
Older adults are at an increased risk of developing pancreatitis. This is likely due to age-related changes in the pancreas and other organs.
Obesity
Obesity is a significant risk factor for pancreatitis. Excess weight puts stress on the pancreas, making it more susceptible to inflammation.
Smoking
Smoking is linked to an increased risk of pancreatitis. Nicotine and other toxins in cigarette smoke can damage the pancreas.
Family History
Having a family history of pancreatitis increases the risk of developing the condition. This suggests a genetic predisposition to pancreatitis.
Summary
Acute pancreatitis is a serious inflammatory condition affecting the pancreas. The most common causes are gallstones and alcohol abuse. Other less common causes include high triglycerides, certain medications, infections, and trauma. Risk factors for pancreatitis include older age, obesity, smoking, and a family history of the condition.
Symptoms of Acute Pancreatitis
Acute pancreatitis is a painful inflammation of the pancreas, an organ that plays a crucial role in digestion. It can occur suddenly and severely, causing a range of symptoms that can vary in intensity from person to person. Understanding the common symptoms of acute pancreatitis is essential for early diagnosis and prompt medical attention.
Common Symptoms
The most common symptoms of acute pancreatitis include:
- Abdominal pain: This is typically the most prominent symptom, often described as a sharp, stabbing pain in the upper abdomen that can radiate to the back. The pain may be constant or intermittent, and it usually worsens after eating, especially fatty foods.
- Nausea and vomiting: Frequent vomiting is common, often accompanied by a feeling of fullness. This can lead to dehydration if not addressed promptly.
- Fever: A temperature above 100.4°F (38°C) is a common sign of inflammation in the pancreas.
- Abdominal tenderness: Pain on palpation of the abdomen is a common finding in acute pancreatitis.
- Other symptoms: Less common symptoms include:
- Jaundice: Yellowing of the skin and whites of the eyes, indicating a problem with the liver or bile ducts.
- Rapid heart rate: A heart rate above 100 beats per minute, which can be a sign of dehydration or shock.
- Low blood pressure: Blood pressure below 90/60 mmHg, which can indicate a problem with blood flow or circulation.
- Shortness of breath: Difficulty breathing, which can occur if the inflammation affects the lungs or causes fluid buildup in the chest.
Pain Associated with Acute Pancreatitis
The pain associated with acute pancreatitis is often described as:
- Location: The pain typically originates in the upper abdomen, often in the middle or slightly to the left. It can radiate to the back, particularly the left side.
- Intensity: The pain can be severe, often rated as 7-10 on a pain scale of 1-10.
- Character: The pain is often described as sharp, stabbing, or burning, and it may be constant or intermittent.
- Triggers: Eating, drinking, or lying down can worsen the pain.
- Relieving factors: Sitting upright or taking pain medication may provide some relief.
Potential Complications of Acute Pancreatitis
Acute pancreatitis can lead to serious complications if left untreated. These complications include:
- Pancreatic Necrosis: This is a life-threatening condition where the pancreatic tissue dies. It can occur when the inflammation becomes severe, causing blood flow to the pancreas to be cut off. Pancreatic necrosis can lead to infection, organ failure, and even death.
- Infection: The pancreas is susceptible to infection when inflammation occurs. These infections can spread to nearby organs or throughout the body, leading to sepsis.
- Fluid Accumulation: Inflammation in the pancreas can cause fluid buildup in the abdomen (ascites) or chest (pleural effusion). This can lead to shortness of breath, abdominal distension, and other complications.
- Organ Failure: Acute pancreatitis can damage other organs, leading to respiratory failure, kidney failure, or liver failure. This is due to the inflammation and toxins released from the pancreas.
- Pseudocyst: A pseudocyst is a collection of fluid that forms in the pancreas. It can occur when the inflammation causes damage to the pancreatic ducts. Pseudocysts can cause pain, pressure on surrounding organs, and infection.
3. Diagnosis of Acute Pancreatitis
Acute pancreatitis is a serious condition that requires prompt diagnosis and treatment. Identifying the cause and severity of the condition is crucial for guiding appropriate management strategies. The diagnostic process involves a combination of clinical assessment, laboratory tests, and imaging studies.
Clinical Presentation of Acute Pancreatitis
The clinical presentation of acute pancreatitis is characterized by a constellation of symptoms and signs. The most common symptom is severe, sudden onset abdominal pain, typically located in the upper abdomen and radiating to the back. The pain is often described as excruciating and persistent.
Other symptoms may include nausea, vomiting, fever, and abdominal distension. Physical examination may reveal signs such as abdominal tenderness, guarding, and rebound tenderness.
Diagnostic Criteria for Acute Pancreatitis
The revised Atlanta classification defines the diagnostic criteria for acute pancreatitis based on clinical, laboratory, and imaging findings. According to this classification, the diagnosis of acute pancreatitis is established when two of the following three criteria are met:
- Abdominal pain consistent with acute pancreatitis
- Serum amylase or lipase levels at least three times the upper limit of normal
- Characteristic findings on imaging studies, such as pancreatic enlargement, peripancreatic fluid collection, or necrosis
Role of Patient History and Physical Examination
The initial assessment of a patient suspected of having acute pancreatitis begins with a thorough history and physical examination. This involves gathering information about the patient’s symptoms, including the onset, duration, and characteristics of abdominal pain, as well as any associated symptoms such as nausea, vomiting, fever, or weight loss.
The physical examination focuses on assessing the abdomen for signs of tenderness, guarding, rebound tenderness, and distension. This information provides valuable clues about the severity and potential causes of the pancreatitis.
Blood Tests in Diagnosing Acute Pancreatitis
Blood tests play a crucial role in confirming the diagnosis of acute pancreatitis and assessing its severity. Several specific blood tests are used to evaluate pancreatic function and identify potential complications.
Amylase and Lipase Levels
Amylase and lipase are enzymes produced by the pancreas that are released into the bloodstream when the pancreas is inflamed. Elevated levels of these enzymes are highly suggestive of acute pancreatitis.
Amylase levels typically rise within 24 hours of the onset of symptoms and peak within 2-3 days. Lipase levels rise more slowly but remain elevated for a longer duration, typically 7-10 days.
While elevated amylase and lipase levels are strong indicators of acute pancreatitis, they are not specific to this condition and can be elevated in other conditions such as bowel obstruction, perforated peptic ulcer, and acute cholecystitis.
Complete Blood Count (CBC)
A complete blood count (CBC) can provide information about the patient’s overall health and identify potential complications associated with acute pancreatitis. In acute pancreatitis, the CBC may show an elevated white blood cell count (leukocytosis), indicating inflammation and infection.
Liver Function Tests (LFTs)
Liver function tests (LFTs) are often performed to assess liver function and identify potential complications of acute pancreatitis. Elevated liver enzymes, such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT), may indicate liver injury or cholestasis, which can occur in acute pancreatitis.
Other Blood Tests
Additional blood tests may be ordered to evaluate specific complications or risk factors for acute pancreatitis. These may include inflammatory markers, such as C-reactive protein (CRP), which can indicate the severity of inflammation, and coagulation tests, such as prothrombin time (PT) and partial thromboplastin time (PTT), to assess the risk of bleeding.
Imaging Techniques in Diagnosing Acute Pancreatitis
Imaging techniques, such as CT scans and ultrasounds, play a crucial role in confirming the diagnosis of acute pancreatitis, assessing its severity, and identifying potential complications.
CT Scans
CT scans provide detailed images of the pancreas and surrounding structures, allowing for the identification of pancreatic enlargement, peripancreatic fluid collection, and necrosis. CT scans are particularly useful for assessing the severity of acute pancreatitis and identifying complications such as pseudocysts, abscesses, and fluid collections.
CT scans are the preferred imaging modality for diagnosing acute pancreatitis and assessing its severity.
However, CT scans expose patients to ionizing radiation, which may be a concern in some cases.
Ultrasounds
Ultrasound is a non-invasive imaging technique that uses sound waves to create images of internal organs. Ultrasound is often used as an initial imaging modality in patients suspected of having acute pancreatitis, especially in pregnant women or those with a history of radiation exposure.
Ultrasound can be used to identify pancreatic enlargement, peripancreatic fluid collection, and other signs of pancreatitis.
However, ultrasound may be limited in its ability to visualize the pancreas in obese patients or those with significant bowel gas.
Diagnostic Approach to Acute Pancreatitis
The diagnostic approach to acute pancreatitis typically involves a combination of clinical assessment, laboratory tests, and imaging studies.
- The initial assessment begins with a thorough history and physical examination to gather information about the patient’s symptoms and clinical presentation.
- Blood tests, including amylase, lipase, CBC, and LFTs, are performed to confirm the diagnosis and assess the severity of pancreatitis.
- Imaging studies, such as CT scans or ultrasounds, are used to visualize the pancreas and surrounding structures, confirm the diagnosis, assess the severity, and identify potential complications.
Treatment of Acute Pancreatitis
Acute pancreatitis is a serious condition, but with timely and effective treatment, most people can recover fully. The primary goal of treatment is to manage pain, prevent complications, and support the body while the pancreas heals.
Pain Management
Pain is a common symptom of acute pancreatitis and can be severe. Effective pain management is crucial for patient comfort and overall well-being. Pain medications, such as opioids, are often prescribed to manage pain, especially during the initial stages of the illness.
Medications and Therapies
Several medications and therapies are used to manage acute pancreatitis and its complications.
- Intravenous Fluids:Dehydration is a common complication of acute pancreatitis, so intravenous fluids are essential to restore hydration and electrolyte balance.
- Antibiotics:If an infection develops, antibiotics are administered to combat the infection and prevent sepsis.
- Proton Pump Inhibitors:These medications help to reduce stomach acid production, which can help prevent complications like ulcers and bleeding.
- Nutritional Support:Patients with acute pancreatitis may need nutritional support through intravenous feeding or a nasogastric tube. This is because the pancreas may not be able to produce enough digestive enzymes to break down food properly.
- Surgery:In some cases, surgery may be necessary to address complications such as abscesses, pseudocysts, or necrotizing pancreatitis.
Complications of Acute Pancreatitis
Acute pancreatitis, while often a temporary condition, can lead to serious complications if left untreated or if the initial attack is severe. These complications can affect various organs and systems, leading to long-term health issues. Understanding these potential complications is crucial for effective management and preventing further damage.
Organ Failure
Organ failure is a major complication of acute pancreatitis. The inflammation in the pancreas can spread to surrounding tissues and organs, affecting their function.
- Respiratory Failure:Inflammation can affect the lungs, leading to fluid buildup and difficulty breathing. This can progress to acute respiratory distress syndrome (ARDS), a serious condition that requires mechanical ventilation.
- Kidney Failure:The pancreas’s inflammation can affect blood flow to the kidneys, leading to acute kidney injury. This can be life-threatening and may require dialysis.
- Cardiac Complications:Acute pancreatitis can cause heart rhythm abnormalities and heart failure, potentially leading to death.
Infections
The inflammatory process in acute pancreatitis can weaken the body’s immune system, making it more susceptible to infections.
- Pancreatic Abscess:A collection of pus forms within the pancreas, requiring surgical drainage.
- Peritonitis:Inflammation spreads to the lining of the abdomen, causing severe pain and requiring immediate medical attention.
- Sepsis:A life-threatening condition where bacteria enter the bloodstream, causing widespread inflammation and organ failure.
Fluid and Electrolyte Imbalances
Acute pancreatitis can lead to fluid and electrolyte imbalances, further complicating the condition.
- Dehydration:The inflammation in the pancreas can cause fluid loss, leading to dehydration and electrolyte imbalances.
- Hypocalcemia:Low calcium levels can occur due to the pancreas’s inability to produce enough calcium-regulating hormones.
Chronic Pancreatitis
Acute pancreatitis can sometimes progress to chronic pancreatitis, a long-term condition characterized by persistent inflammation and damage to the pancreas. This can lead to ongoing pain, digestive problems, and malnutrition.
Long-Term Consequences
Acute pancreatitis can have long-term consequences, even after the initial attack has subsided.
- Diabetes:Damage to the pancreas can affect its ability to produce insulin, leading to diabetes.
- Malnutrition:The pancreas’s role in digestion is compromised, leading to difficulty absorbing nutrients and causing malnutrition.
- Pain:Chronic pain is a common long-term consequence of acute pancreatitis, often requiring pain management strategies.
6. Prevention of Acute Pancreatitis: A Student Learns What Information About Acute Pancreatitis

While there’s no foolproof way to prevent acute pancreatitis, adopting healthy lifestyle habits can significantly reduce your risk. Understanding the causes and risk factors can empower you to make informed choices for your well-being.
Lifestyle Modifications for Prevention
Making changes to your lifestyle can play a crucial role in preventing acute pancreatitis. These modifications focus on reducing the factors that can trigger the condition.
- Limit Alcohol Consumption:Excessive alcohol intake is a major contributor to pancreatitis. Reducing or eliminating alcohol consumption is highly recommended.
- Reduce Fat Intake:A diet high in saturated and trans fats can strain the pancreas. Opt for lean protein sources, fruits, vegetables, and whole grains.
- Maintain a Healthy Weight:Obesity is a risk factor for pancreatitis. Maintaining a healthy BMI through a balanced diet and regular exercise is important.
- Avoid Smoking:Smoking damages the pancreas and increases the risk of pancreatitis. Quitting smoking is essential for overall health and pancreas health.
- Regular Exercise:Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week.
Role of Early Diagnosis and Treatment of Underlying Conditions
Promptly identifying and managing underlying conditions that increase the risk of pancreatitis is vital.
Learning about acute pancreatitis can be a lot to take in, especially if you’re a student. It’s important to figure out how you learn best, whether you’re a visual learner who thrives on diagrams and pictures, a kinesthetic learner who prefers hands-on activities, or maybe you’re an auditory learner who excels with lectures and discussions.
What’s your learning style is an appropriately worded question to ask yourself, as it can help you find the best way to absorb all the information about acute pancreatitis. Once you understand your learning style, you can tailor your study methods and make the process a lot easier!
- Gallstones:Gallstones can block the bile duct, leading to pancreatitis. Surgical removal of gallstones can prevent this complication.
- Alcohol Abuse:Alcohol cessation is crucial for individuals with alcohol-related pancreatitis.
- High Triglycerides:Medications to lower triglyceride levels can reduce the risk of pancreatitis in individuals with hypertriglyceridemia.
Key Preventive Measures
A holistic approach to preventing acute pancreatitis involves lifestyle changes, early diagnosis, and effective management of underlying conditions. Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding alcohol and smoking, is essential. Early detection and treatment of risk factors like gallstones, alcohol abuse, and high triglycerides can significantly reduce the likelihood of developing pancreatitis.
It’s crucial to consult with your healthcare provider for personalized guidance and management of any potential risk factors.
Prognosis of Acute Pancreatitis
The prognosis of acute pancreatitis, or the expected outcome, depends on several factors, including the severity of the inflammation, the presence of complications, and the overall health of the individual. Early diagnosis and prompt management play a crucial role in improving the chances of a favorable outcome.
Factors Influencing Prognosis
The severity of acute pancreatitis is often categorized using a scoring system like the Ranson criteria or the APACHE II score. These scores consider factors such as age, blood sugar levels, white blood cell count, and the presence of complications.
Higher scores indicate a more severe case with a poorer prognosis.
- Severity of Pancreatitis:As mentioned, the severity of the pancreatitis is a major determinant of prognosis. Mild cases often resolve with conservative treatment, while severe cases may lead to complications and require intensive care.
- Presence of Complications:Complications such as pancreatic necrosis, infection, or organ failure significantly worsen the prognosis. Early identification and management of complications are crucial for improving survival rates.
- Underlying Medical Conditions:Individuals with pre-existing medical conditions, such as diabetes, heart disease, or chronic kidney disease, may have a higher risk of complications and a poorer prognosis.
- Age:Older adults and children may have a higher risk of complications and a poorer prognosis compared to younger adults.
- Alcohol Consumption:Chronic alcohol abuse is a major risk factor for pancreatitis and can contribute to a poorer prognosis.
- Nutritional Status:Malnutrition can weaken the body’s ability to fight infection and recover from pancreatitis, impacting the prognosis.
Importance of Early Intervention and Management
Prompt medical attention and appropriate management are crucial for improving the prognosis of acute pancreatitis. Early diagnosis allows for timely interventions, such as intravenous fluids, pain management, and nutritional support, which can help prevent complications and promote recovery.
Long-Term Outlook
The long-term outlook for individuals with acute pancreatitis varies depending on the severity of the initial attack and the presence of complications.
- Mild Cases:Individuals with mild pancreatitis typically recover fully without long-term consequences.
- Severe Cases:Individuals who experience severe pancreatitis may develop chronic pancreatitis, which can lead to persistent pain, digestive problems, and an increased risk of pancreatic cancer.
- Complications:The presence of complications, such as pancreatic necrosis or infection, can significantly impact the long-term outlook. These complications may require ongoing medical management and can increase the risk of long-term health issues.
Role of Nutrition in Acute Pancreatitis
Acute pancreatitis is a serious condition that can lead to significant complications, including malnutrition. Proper nutritional support is crucial during the acute phase of pancreatitis to ensure adequate healing and recovery. This section will discuss the importance of nutrition in managing acute pancreatitis, providing dietary recommendations for different phases of the disease, and offering guidance on how to manage nutritional needs long-term.
Importance of Nutritional Support, A student learns what information about acute pancreatitis
Nutritional support is essential during the acute phase of pancreatitis for several reasons. Firstly, the inflamed pancreas is unable to produce digestive enzymes effectively, leading to maldigestion and malabsorption of nutrients. This can result in a significant loss of calories, protein, and essential vitamins and minerals.
Secondly, the body’s response to inflammation during acute pancreatitis can lead to increased metabolic demands, requiring additional energy and nutrients for healing and tissue repair. Inadequate nutritional intake during this phase can exacerbate the inflammatory process, delay healing, and increase the risk of complications.
Dietary Recommendations for Acute Pancreatitis
Dietary modifications are essential during the acute phase of pancreatitis to minimize stress on the inflamed pancreas and promote healing.
Fluid Intake
Adequate hydration is crucial during the acute phase to prevent dehydration, which can worsen the condition. Clear fluids, such as water, broth, and diluted fruit juices, are recommended initially. As the patient’s condition improves, they can gradually transition to other fluids like milk and yogurt.
Calorie Restriction
Calorie restriction is often necessary in the acute phase to reduce the workload on the pancreas. The goal is to provide enough calories to meet the body’s basic energy needs while minimizing the production of digestive enzymes. The amount of calorie restriction will vary depending on the individual’s needs and the severity of the pancreatitis.
Fat Intake
Fat restriction is essential during the acute phase to reduce the burden on the pancreas. Fats are the primary stimulus for pancreatic enzyme production, so limiting fat intake can help reduce inflammation and pain. High-fat foods, such as fried foods, fatty meats, and dairy products, should be avoided.
Protein Intake
Adequate protein intake is essential for tissue repair and wound healing. Lean protein sources, such as fish, chicken, beans, and tofu, are recommended.
Sample Meal Plan
Here is a sample meal plan for a patient with acute pancreatitis: Breakfast:Oatmeal with berries and skim milk Lunch:Grilled chicken salad with mixed greens and a light vinaigrette dressing Dinner:Baked salmon with steamed vegetables
Managing Nutritional Needs During Recovery
As the acute phase subsides, the patient can gradually transition to a more liberal diet. The goal is to reintroduce food groups gradually while monitoring for any signs of intolerance or discomfort.
Transition to a More Liberal Diet
During the recovery phase, the patient can gradually increase their calorie and fat intake. It is important to start with small, frequent meals and avoid large, fatty meals.
Long-Term Nutritional Management
Long-term nutritional management may involve ongoing dietary modifications and the use of supplements. A registered dietitian can provide personalized recommendations based on the individual’s needs and medical history.
Regular Follow-up
Regular follow-up with a healthcare professional is crucial to monitor nutritional status and adjust dietary recommendations as needed.
Patient Education and Support
Patient education and support are essential for individuals diagnosed with acute pancreatitis. Understanding the condition, its management, and potential complications empowers patients to actively participate in their care and improve their overall well-being.
Importance of Patient Education and Support
Providing patients with comprehensive information about acute pancreatitis helps them make informed decisions regarding their treatment and lifestyle modifications. Effective communication between healthcare professionals and patients fosters trust and encourages adherence to recommended therapies. Support groups and online resources offer valuable connections with others who have experienced similar challenges, promoting emotional well-being and reducing feelings of isolation.
Key Information for Patients
Patients should be aware of the following key aspects of acute pancreatitis:
- Causes and risk factors:Understanding the causes of acute pancreatitis, such as gallstones, alcohol abuse, and certain medications, allows patients to identify and manage potential risk factors.
- Symptoms:Recognizing the typical symptoms of acute pancreatitis, including severe abdominal pain, nausea, vomiting, and fever, enables early diagnosis and prompt medical attention.
- Diagnosis and treatment:Patients should be familiar with the diagnostic procedures used to confirm acute pancreatitis, such as blood tests, imaging studies, and endoscopy. They should also understand the various treatment options, including pain management, fluid replacement, and nutritional support.
- Complications:Awareness of potential complications, such as infection, organ failure, and chronic pancreatitis, helps patients understand the importance of adhering to treatment plans and seeking immediate medical attention if complications arise.
- Lifestyle modifications:Patients should be educated about lifestyle changes that can reduce their risk of developing acute pancreatitis, such as avoiding alcohol consumption, maintaining a healthy weight, and managing underlying medical conditions.
- Prognosis and long-term management:Understanding the prognosis of acute pancreatitis and the potential for long-term complications helps patients make informed decisions about their ongoing care and lifestyle choices.
Role of Healthcare Professionals
Healthcare professionals play a vital role in providing guidance and support to patients with acute pancreatitis.
- Clear communication:Healthcare professionals should communicate effectively with patients, using clear and understandable language to explain the condition, treatment options, and potential risks and benefits.
- Personalized care:Healthcare professionals should tailor their approach to individual patients, considering their specific needs, preferences, and cultural background.
- Emotional support:Healthcare professionals should provide emotional support to patients, acknowledging the challenges they may face and offering resources to help them cope with stress and anxiety.
- Referral to specialists:Healthcare professionals should refer patients to appropriate specialists, such as gastroenterologists or surgeons, for specialized care and management of acute pancreatitis.
- Follow-up care:Healthcare professionals should provide ongoing follow-up care to monitor patients’ progress, adjust treatment plans as needed, and address any concerns or questions.
Research and Future Directions
Acute pancreatitis is a complex disease with significant morbidity and mortality. Ongoing research aims to improve our understanding of the disease, develop more effective treatments, and ultimately reduce the burden of this condition.
Clinical Trials and Patient Outcomes
Clinical trials play a crucial role in advancing our understanding of acute pancreatitis and improving patient outcomes. These trials evaluate the effectiveness and safety of new treatments, such as novel medications or surgical techniques. By participating in clinical trials, patients contribute to the development of new therapies and help to ensure that future generations receive the best possible care.
For example, a recent clinical trial investigated the use of a new drug called [Drug Name] for the treatment of severe acute pancreatitis. The trial found that [Drug Name] was associated with a significant reduction in mortality and complications compared to standard treatment.
FAQ Guide
What is the most common symptom of acute pancreatitis?
Abdominal pain is the most common symptom of acute pancreatitis. It’s often described as a sharp, stabbing pain in the upper abdomen that can radiate to the back.
Is acute pancreatitis contagious?
No, acute pancreatitis is not contagious. It’s caused by inflammation of the pancreas, which is not transmitted from person to person.
Can acute pancreatitis be prevented?
Yes, there are steps you can take to reduce your risk of developing acute pancreatitis. These include maintaining a healthy weight, limiting alcohol consumption, and managing underlying conditions like gallstones.
What are the long-term consequences of acute pancreatitis?
Long-term consequences of acute pancreatitis can vary depending on the severity of the condition and the presence of complications. Some individuals may experience chronic pancreatitis, while others may have ongoing digestive issues or require long-term management of complications like diabetes or pancreatic insufficiency.
